
Analyzing the Immediate Effects of Joint Mobilizations on Muscular Strength
May 2025

When most people think about increasing muscle strength, they picture barbells, reps, and progressive overload. At PFP, we are strength and conditioning coaches at heart, but what if we told you that strength can sometimes be unlocked not by adding load, but by freeing a joint?A capstone project completed by the Class of 2025 and soon-to-be Doctors of Physical Therapy (DPT) students at New York Medical College constructed a systematic review that examined the immediate effects of joint mobilizations on muscular strength. Don’t worry, this will not be a beefy research paper; but we will summarize the key points and gold nuggets for you!
Before we continue... Shout out to my classmates, research group members, and soon-to-be DPT's who I worked with on this capstone project:Dr. Daisy Alvarez
Dr. Alexander Morales
Dr. Frank Schultz
Dr. Yue Tang
Dr. Rommel Torres

What Is A Joint Mobilization?
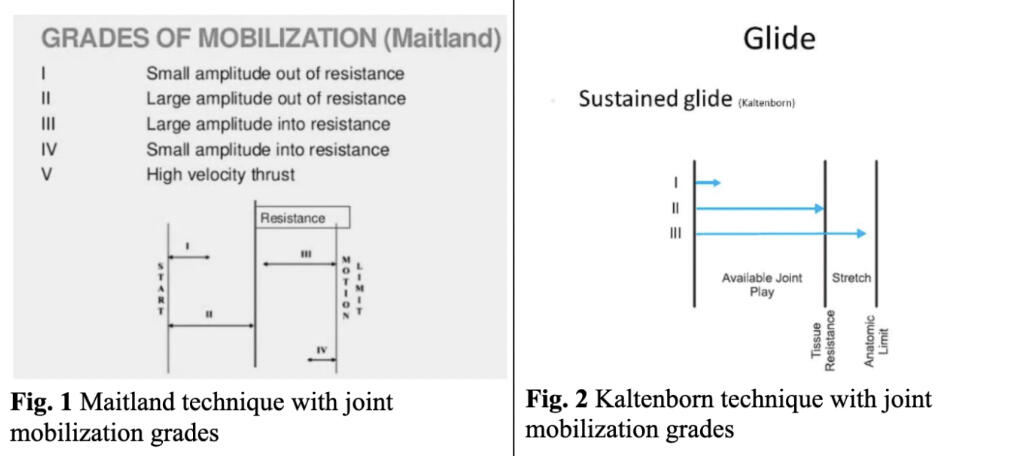
Joint mobilizations are passive, skilled manual therapy techniques that apply graded passive movements to a joint, which subsequently influences the surrounding soft tissue structures. These techniques fall on a spectrum based on amplitude and velocity, with different schools of thought.1) Maitland mobilizations (Grades I–V): Rhythmic oscillations used for pain modulation and capsular / joint mobility.2) Kaltenborn techniques: Sustained glides for joint traction and capsular stretch.3) HVLA (High Velocity, Low Amplitude AKA Maitland Grade V) thrusts: Quick manipulations applied at the end range to restore joint mechanics.4) Mulligan’s Mobilization with Movement (MWM): Combines therapist-applied glides with active, pain-free movement from the patients
These aren’t just “cracks” or “wiggles” typically associated with the term manipulations. When applied with purpose and clinical reasoning, they create measurable neurophysiological and mechanical changes, and they may just be the key to unlocking underperforming muscle groups.

Here are the leading mechanistic theories how joint mobilizations can lead to immediate improvements in force production of the surrounding musculature:
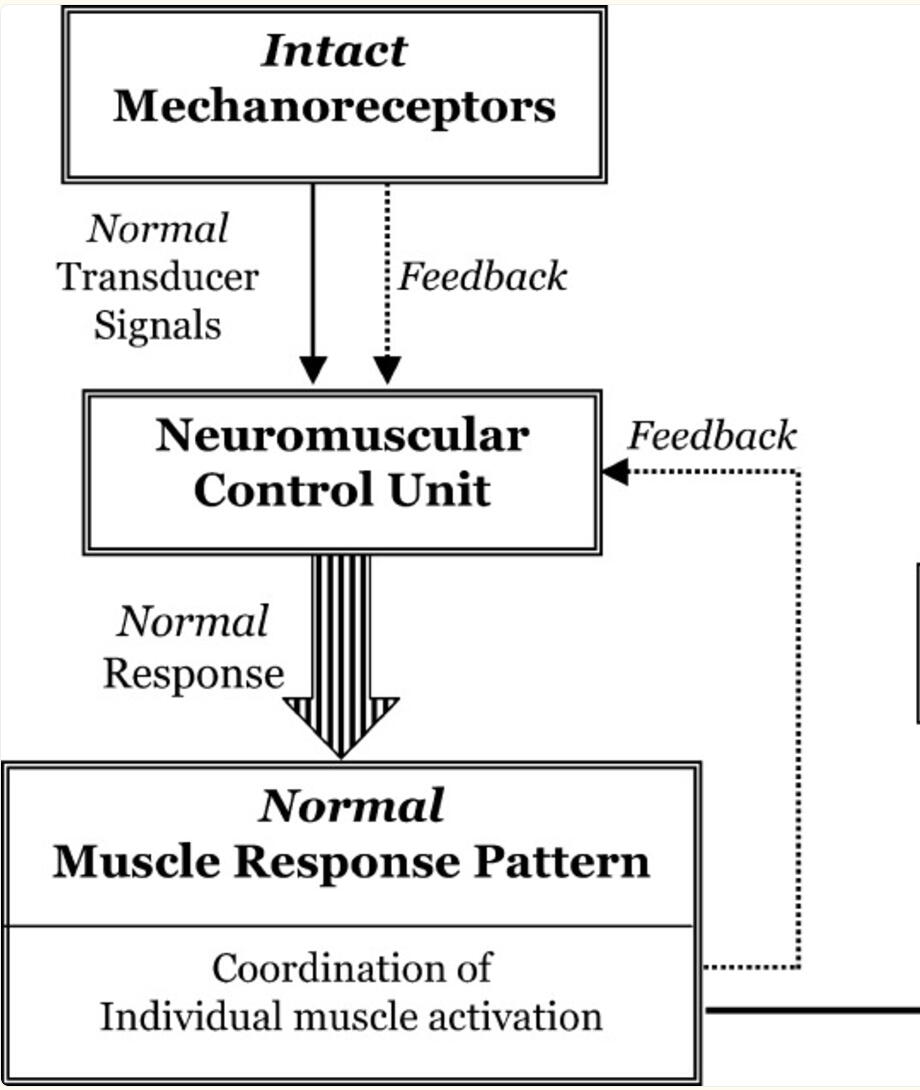
1. Arthrokinetic Reflex (AKR) and Neuromuscular FacilitationAKR is a spinal-level reflex first explored in the 1950’s. When joint mobilizations are performed, joint mechanoreceptors stimulation and reflexive muscle contraction of the surrounding muscles occur in response (Makofsky et al., 2007). The AKR also modulates the excitability of alpha motor neurons of the surrounding muscles Fisher et al., 2016; Motealleh et al., 2016). This in turn can lead to increased motor unit recruitment (more action signals sent to the muscles to fire and to contract) Fisher et al., 2016; Motealleh et al., 2016) while also reducing inhibitory signals from the brain.In practical terms: if your joint is hypomobile or dysfunctional, the local muscle(s) may be neurologically inhibited. Mobilizing the joint restores normal proprioceptive input, decreasing inhibition, and increasing muscle firing.
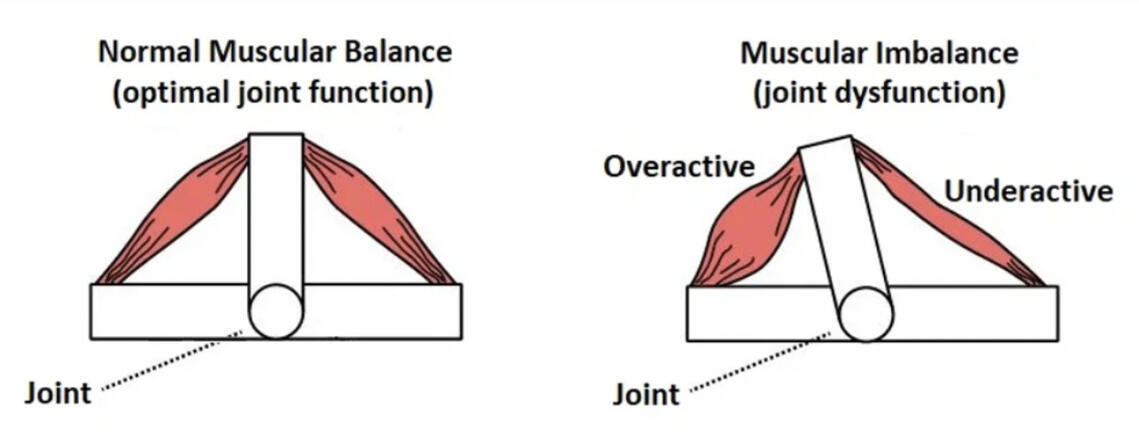
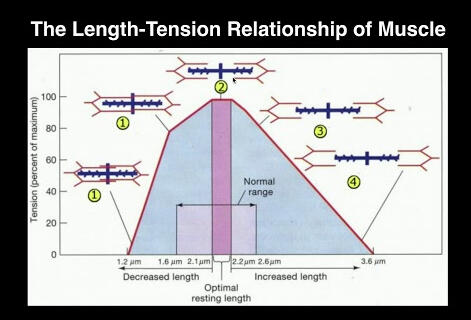
2. Mechanical & Biomechanical EfficiencyPoor joint mechanics = poor leverage. By restoring normal joint mechanics and relative motions, you improve the length-tension relationship of surrounding muscles. When a muscle is too long or too short, its efficiency in producing force is dampened. If there is an optimal joint position, the muscle has relatively “normal” resting length, which ultimately allows the muscles to contract from a more mechanically advantageous position — improving torque and force output.
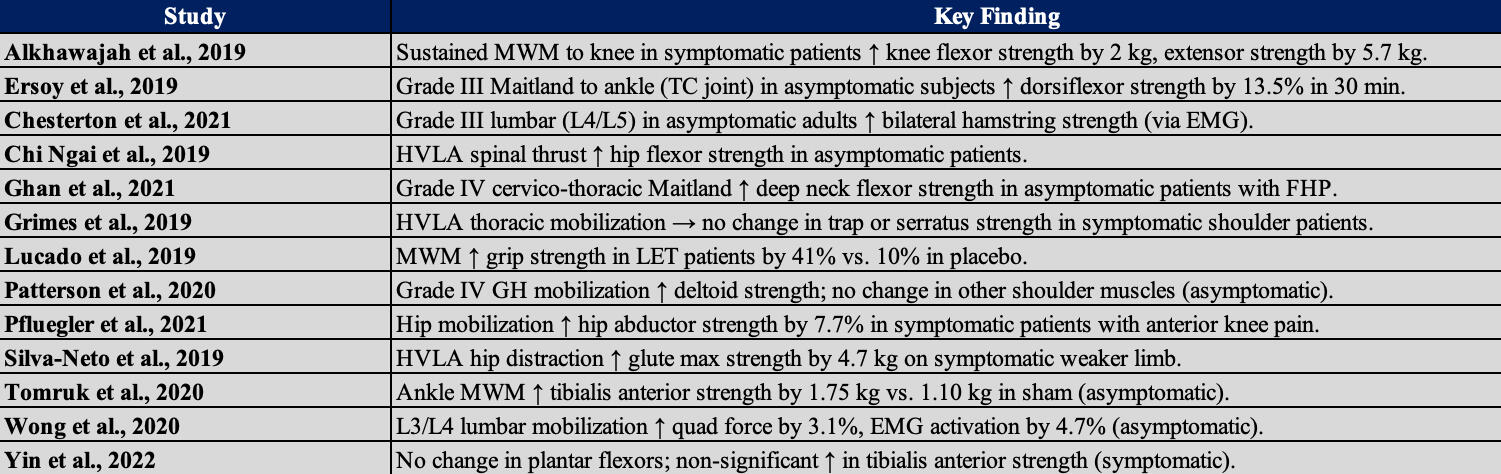
What the Research Shows:Our research capstone project found 13 high-quality studies that fit our inclusion criteria: studies from 2019 onward, with symptomatic and asymptomatic patients, using objective strength measurements (handheld dynamometry, EMG, isokinetic dynamometers), with a comparison or control group, and changes in strength of local muscles measured within 24 hours of the intervention.See the table for the KEY findings for each study
Collectively, these studies show that joint mobilizations have a much greater impact than just manipulating the joint position — it has the potential to influence neuromuscular function, enhancing local muscle strength and force output.
Clinical ImplicationsEvidence suggests that joint mobilizations, regardless of technique, can acutely improve muscle strength (Alkhawajah et al., 2019; Chesterton et al., 2021; Chi Ngai et al., 2019; Ersoy et al., 2019; Ghan et al., 2021; Lucado et al., 2019; Pfluegler et al., 2021; Silva-Neto et al., 2019; Tomruk et al., 2020; Wong et al., 2020; Yin et al., 2022); however, inconsistent protocols and varying methodologies across studies limit the ability to draw definitive clinical guidelines. This lack of standardization highlights the pressing need for standardized protocols in musculoskeletal therapy.Lastly, inherent subjectivity in the application of joint mobilizations, particularly in regard to the grading of Maitland mobilizations, must be addressed. Differences in clinician skill, perception, and force application can result in inconsistent grading, even when following established guidelines. For example, what one PT considers a Grade III mobilization, another might not. These discrepancies can affect outcome reliability and should be accounted for in both clinical practice and future research.


Takeway:While joint mobilization shows real potential for enhancing muscle strength, current research lacks uniform protocols, making widespread clinical recommendations premature. Until more standardized protocols are established, clinicians should tailor joint mobilization interventions to each patient, considering the joint involved, symptom presentation, and the clinician's own experience with the technique.In conclusion, joint mobilization is promising, but until protocols are standardized, its use should remain individualized and evidence-informed. Future research must focus on reproducible methods to strengthen both outcomes and confidence in this intervention.